Painting a More Complete Picture of WIC: How WIC Impacts Nonparticipants
- by Victor Oliveira and Elizabeth Frazão
- 4/6/2015
Highlights
- Requirements that WIC-authorized stores stock a minimum variety and quantity of WIC foods increases availability of healthy foods in some small WIC and non-WIC stores.
- To qualify as WIC-eligible, some foods had to be reformulated, which has increased the nutrient quality of some foods purchased by WIC and non-WIC customers.
- WIC program regulations may have had the unintended effect of raising prices and limiting availability of non-WIC brands of infant formula in some retail food stores.
The Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) helps safeguard the health of nutritionally at risk low-income pregnant, breastfeeding, and postpartum women, as well as infants and children younger than 5 years of age, by providing a package of supplemental foods, nutrition education, and referrals to health care. With Federal expenditures of over $6 billion in fiscal 2014, WIC is the Nation’s third-largest food and nutrition assistance program, trailing only the Supplemental Nutrition Assistance Program (SNAP) and the National School Lunch Program.
The Healthy, Hunger-Free Kids Act of 2010, which authorized funds for WIC, is set to expire on September 30, 2015. The reauthorization process provides policymakers an important opportunity to reexamine the operation and effectiveness of the program and consider improvements. To fully evaluate the program, it is important to account for all the program’s effects—direct and indirect, intended and unintended, positive as well as negative. A comprehensive 2012 review of WIC research conducted for USDA’s Food and Nutrition Service—the agency responsible for administering the program—concluded that WIC participation directly impacts the health and nutrition of participants through improved diets (including increased iron density, fewer added sugars, and a greater variety of foods) and greater use of health care services.
WIC can also indirectly impact the food choices, diet, and health of nonparticipants, through its effects on retail food stores and food manufacturers. In general, these impacts have previously received little attention. To paint a more complete picture of WIC, ERS researchers looked at some of the indirect effects of WIC on nonparticipants.
Food Packages Are the Cornerstone of WIC
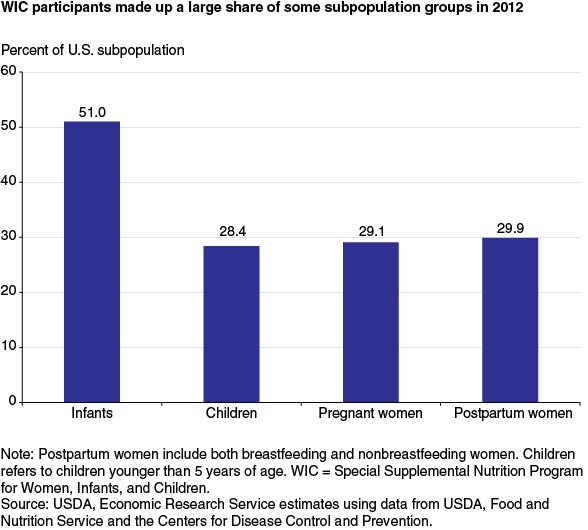
An average of 8.9 million people participated in WIC each month in fiscal 2012, including over half of all infants in the United States, and over a quarter of all pregnant and postpartum women and children up to age 5. WIC offers participants supplemental food packages containing specific types and quantities of foods tailored to the nutritional needs of the program’s target population. The food packages accounted for over two-thirds of total WIC costs in fiscal 2014. Most WIC participants obtain their WIC foods by exchanging a voucher, check, or electronic benefit card at over 47,000 WIC-authorized retail food stores that are required to stock minimum varieties and quantities of WIC foods. State WIC agencies reimburse the retail vendors—which include supermarkets, grocery stores, mass merchandisers, and convenience stores—for the food purchased through WIC.
One of the most important changes in the program’s 40-year history occurred in 2007, when the program revised both the types and amounts of food included in the program’s food packages. Prior to the revisions, WIC foods included infant formula, milk, infant cereals, breakfast cereals, juice, cheese, eggs, peanut butter, dried and canned beans/peas, and canned fish. The revisions—implemented in 2009—included the addition of fruits and vegetables and whole-wheat bread, required that at least half of all breakfast cereals allowed be whole-grain, added several culturally appropriate substitutes (such as whole-grain tortillas or brown rice for the whole-wheat bread), and restricted the fat content of milk to 1% or lower for most participants.
WIC Impacts Nonparticipants by Increasing Availability of Healthy Foods at Small Food Stores…
As a result of the revisions to the WIC food packages, WIC-authorized vendors are required to stock at least two varieties of fruits, two varieties of vegetables, one whole-grain cereal, and lower fat milk. In order to maintain their WIC authorization, some vendors—in particular smaller stores—had to expand the types and quantities of food items they stocked. As expected, research indicates that the availability of healthy foods (proxied by the newly added WIC foods) in small WIC-authorized stores increased after the food package revisions were implemented.
One study of convenience stores and nonchain grocery stores in five towns in Connecticut found that the healthy food supply score (based on availability, variety, prices of healthy foods, and produce quality) increased 39 percent in WIC convenience and grocery stores in lower income neighborhoods, and 16 percent in WIC convenience and grocery stores in higher income neighborhoods. Because WIC-authorized stores serve both WIC and non-WIC customers, the improved availability of healthy foods in these stores increased access to healthy foods for the entire community, not just for WIC participants.
An unintended consequence of WIC’s stocking requirement was the increased availability of healthy foods in non-WIC convenience and grocery stores, which are not required to stock the new WIC foods. The healthy food supply score in small non-WIC stores increased 4 percent. Researchers attribute this increase to competition with WIC-authorized stores as well as improved distribution chains resulting from suppliers—who serve both WIC-authorized and non-WIC stores—carrying the new WIC foods. This suggests the potential for a beneficial spillover effect on non-WIC households regardless of whether they shop at WIC-authorized stores or other stores. Increased local access to healthy foods could have beneficial long-term impacts on diet quality and health among both WIC and non-WIC households.
... and by Affecting Availability and Price of Infant Formula
Not all of WIC’s impacts on nonparticipants are positive. By providing low-income families with free formula, WIC essentially replaces price-sensitive consumers of infant formula with price-insensitive consumers, thereby providing an incentive to both manufacturers and retailers to increase their prices. ERS has estimated that well over half of all infant formula sold in the United States is purchased through WIC. To reduce costs to WIC, Federal law requires that WIC State agencies enter into cost-containment contracts with manufacturers of infant formula. Typically, infant formula manufacturers compete for each State’s infant formula contract which gives the winning manufacturer the exclusive right to provide its products to WIC participants in the State. In exchange, WIC State agencies obtain substantial discounts in the form of rebates from the formula manufacturer for each can of formula purchased through the program (see box “WIC Participants Supported by Rebates”). As a result, the brand of formula provided by WIC varies by State, depending on which manufacturer holds the contract.
An ERS-funded study suggests that wholesale prices of infant formula—adjusted for inflation—have doubled over what they would have been in the absence of WIC and its rebate program. Another ERS study found that, for a given set of wholesale prices, WIC and its rebate program resulted in modest increases in the supermarket price of the WIC brand of infant formula —about 2.5 cents per 26 reconstituted ounces of formula in 2000 dollars (or about 1 percent of the retail price). Furthermore, as the number of WIC formula-fed infants increased relative to the number of non-WIC formula-fed infants in a State, prices in supermarkets increased for both the WIC and the non-WIC brands of formula. Researchers found that the monthly cost of formula-feeding a 3-month old girl increased between $0.32 and $5.26 for families that lived in an area where WIC participation was significantly higher than the national average. Together, these studies suggest that WIC and its infant formula rebate program result in higher formula prices for non-WIC consumers, thereby impacting the food budgets of non-WIC families with formula-fed infants.
WIC’s rebate program may also negatively affect the variety of infant formula brands available in stores. Given that WIC stores are required to maintain a minimum stock of the WIC brand of formula, it may not make financial sense for retailers to devote valuable shelf space to non-WIC brands. This may be especially true for smaller stores with limited shelf space. These stores may decide to stock only the biggest seller, which in most cases will be the WIC brand. Non-WIC patrons of these stores may choose to purchase the WIC-brand of formula at that store rather than travel to another store to purchase non-WIC brands of formula.
WIC Also Affects Nonparticipants Through Its Effects on Food Producers
WIC regulations regarding the nutrient content and packaging of WIC foods and policies governing WIC’s infant formula rebate program have been shown to impact some food producers, which can in turn improve the availability of healthy foods for nonparticipants. For example, WIC requires that all cereals provided through the program be fortified with iron. Some manufacturers may feel that WIC children represent a potentially lucrative market, since WIC children who grow up consuming a particular brand of WIC cereal may develop a preference for that product that extends past their time in the program and have responded by reformulating some of their products. In 1985, General Mills increased the amount of iron in Cheerios—one of the most popular WIC-eligible cereals—so that it would meet program requirements. Today, manufacturers produce a large number of cereal products that meet WIC’s requirements—cereals purchased and consumed by both WIC and non-WIC participants. On the other hand, some manufacturers lobby to change WIC regulations (see box “Food Producers Lobby to Change WIC Foods”).
By requiring that all infant formula and all infant cereals and breakfast cereals provided through WIC be fortified with iron, WIC has had a direct effect on reducing the prevalence of anemia among participating children. The prevalence of anemia among low-income children declined from almost 8 percent in 1975 (when WIC was just starting) to less than 3 percent in 1985. Because these iron-fortified products were also available to—and consumed by—non-WIC individuals, WIC is credited with reducing iron-deficiency anemia among non-WIC children as well.
The addition of whole-wheat bread to the WIC food packages in 2009 provides another example of how nonparticipants can be indirectly impacted by WIC’s effects on manufacturers. The recent WIC food package revisions added 1 pound of whole-wheat bread to the food packages for pregnant and breastfeeding women, and 2 pounds to the food package for children. Since bread is most commonly sold in 24-ounce loaves, some believed that WIC participants might have difficulty finding 16-ounce loaves of whole-wheat bread at retail stores, making it difficult for participants to purchase the maximum monthly allowances. However, anecdotal evidence suggests that bread manufacturers responded to the need for a new package size as whole-wheat bread in the authorized package sizes is now available in all States. Anecdotal evidence further suggests that some non-WIC individuals—for example seniors living alone—prefer the smaller package size.
WIC policies have had especially large repercussions in the infant formula market. In the early 2000s, infant formula manufacturers introduced formulas supplemented with the fatty acids docosahexaenoic acid (DHA) and arachidonic acid (ARA), which some studies have linked to improved vision and cognitive development in infants. Under provisions in the Child Nutrition and WIC Reauthorization Act of 2004, the decision of which infant formula product is offered as first choice to WIC participants in the State depends on which product the winning manufacturer uses to bid for the WIC contract (previously, WIC State agencies specified the product to be used in the bid). Manufacturers have chosen to use the significantly higher priced supplemented formulas in their bids. As a result, WIC participants were provided these new supplemented formulas.
Since the WIC brands of formula account for over half of all infant formula sales in the United States, the legislation in effect guaranteed large sales volumes for the newly introduced supplemented formula products, thereby increasing their visibility in retail stores to non-WIC consumers, and expediting the demise of unsupplemented infant formula in the marketplace. Sales of DHA/ARA-supplemented formulas now account for nearly all sales of infant formula in the United States.
WIC Impacts the Diets of Nonparticipating Children in WIC Families
An ERS study examined whether the benefits of WIC participation extended to older (and therefore ineligible) children in WIC families. The study showed that nonparticipating children in WIC families scored higher on the Healthy Eating Index (HEI, a measure of diet quality that assesses conformance to Federal dietary guidance) than similarly aged children in non-WIC families. This association was stronger for children in families with two or more WIC participants compared with children living with only one or no WIC participants, suggesting that a larger dose of WIC benefits had a larger impact on the diets of other children in the family.
These findings do not necessarily mean that WIC benefits are being shared with nonparticipating children. This result could occur if the nutrition education that WIC participants receive impacts the diets of other family members; for example, if the WIC participant uses what was learned in WIC to prepare healthy meals for the entire family. A higher HEI could also occur if the benefits of WIC participation have an income effect, whereby the money that would otherwise have been used to buy food for the WIC participant is now spent on other foods that affect the diets of nonparticipating family members.
Although WIC is narrowly targeted to low-income pregnant and postpartum women, infants, and preschool children, its impacts can be felt across all income levels and population groups. WIC has been shown to increase the availability of healthy foods in small stores and impact the nutrient composition and food package sizes of certain foods. As a result, WIC has contributed to increased access to healthy foods, increased food options, and improved diet quality among both participants and nonparticipants. On the other hand, WIC may also raise the price and limit the availability of some brands of infant formula in retail food stores. Accounting for all of WIC’s effects—on both participants and nonparticipants—is important to accurately gauge the impact of potential changes to the program.
This article is drawn from:
- Oliveira, V. & Frazão, E. (2015). The WIC Program: Background, Trends, and Economic Issues, 2015 Edition. U.S. Department of Agriculture, Economic Research Service. EIB-134.
You may also like:
- Oliveira, V., Frazão, E. & Smallwood, D. (2011). The Infant Formula Market: Consequences of a Change in the WIC Contract Brand. U.S. Department of Agriculture, Economic Research Service. ERR-124.
- 'Do Benefits of U.S. Food Assistance Programs for Children Spillover to Older Children in the Same Household?,' by M. Ver Ploeg. (2009). Journal of Family and Economic Issues Vol. 30(4).
- “Positive Influence of the Revised Special Supplemental Nutrition Program for Women, Infants, and Children Food Packages on Access to Healthy Foods,” by T. Andreyeva, J. Luedicke, A.E. Middleton, M.W. Long, and M.B. Schwartz. (2012). Journal of the Academy of Nutrition and Dietetics, 112: 850-858.