Obesity Policy and the Law of Unintended Consequences
- by Fred Kuchler, Elise Golan, Jay Variyam and Steve Crutchfield
- 6/1/2005
Americans are increasingly overweight, with the number of obese adults and overweight children doubling between the late 1970s and early 2000s. Several studies of the health consequences of Americans’ weight gain indicate that health care costs and the number of premature deaths associated with obesity and overweight are high. A recent (lower) estimate of the number of premature deaths published in the Journal of the American Medical Association reveals the uncertainty researchers face in associating weight status with mortality. Of course, scientific uncertainty does not mute demands for public action.
Action to combat obesity and overweight could come in many forms since many variables influence diet and lifestyle choices. While economics tells us that prices and income shape choices, other factors are important, too. Individuals choose foods based on taste, convenience, family structure and traditions, age, health status, knowledge, and lifestyle. Policy targeted at any of these factors could have some success in reducing obesity and overweight. However, such success is likely to be limited if all other factors remain unchanged. The economic levers available to policymakers to create incentives for individuals to alter diet and lifestyle choices affect only some of the determinants of food choices.
The wide range of factors contributing to food choices is compounded by the incredible variety of foods and consumption opportunities available today—we make choices among thousands of food products, choices about whether to eat at home or in a variety of restaurants, and choices about lifestyles, such as diet quality and exercise. As a result of nearly unlimited choice, public policy targeting specific foods or lifestyle choices could have surprising unintended consequences. ERS has examined some of the potential intended and unintended consequences of three widely discussed obesity policies—nutrition labels in restaurants, taxes on snack foods, and restrictions on food advertising to children—with a focus on the likely effect of each program on producer and consumer incentives and on health outcomes. In every case, the unintended effects could dampen the policy’s success in reducing overweight and obesity.
Nutrition Labeling at Restaurants
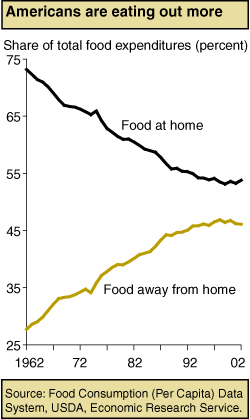
The 1994 National Labeling and Education Act (NLEA) requires manufacturers to include a nutrition information panel on the label of almost all packaged foods, but it does not require any similar disclosure for foods purchased at restaurants—food-away-from-home (FAFH). The lack of nutrition information for FAFH means that if consumers misjudge the nutrient content of meals eaten out, they may inadvertently overconsume some nutrients and underconsume others. An ERS study showed that FAFH typically contained more of the nutrients overconsumed (fat and saturated fat) and less of the nutrients underconsumed (calcium, fiber, and iron) by Americans. Because FAFH commands a large and increasing share of total food expenditures, nutrition choices at FAFH could have a large effect on overall diet quality.
If consumers choose high-fat or high-calorie foods because they lack FAFH nutrition information, then mandatory FAFH labeling could potentially lead to improvements in consumers’ food choices and health. However, lack of information may not be the reason for poor nutritional FAFH choices, either because the industry supplies enough information or consumers deduce the information (see “Is There Evidence That Obesity and Overweight Are the Result of Market Failure?”). In such cases, making standardized nutrition labels mandatory for major sources of FAFH such as fast food and chain restaurants will not improve public health.
Recent consumer choice studies suggest that the effect of nutritional information on diet in FAFH settings may be modest. For example, a Pennsylvania State University study of food intake among normal-weight women found that explaining the concept of energy density (amount of calories per gram of food) and providing nutrition information on labels during meals in a laboratory setting had no impact on subjects’ energy intakes. A restaurant study in England found that providing nutrition information had no effect on overall energy and fat intake of patrons. In fact, the presence of “lower fat” information was associated with fewer restaurant patrons’ selecting the target dish. Another study in an Army cafeteria found no significant difference between sales before and after nutrition labeling for either average “healthy” (labeled, containing less than 15 grams of fat and 100 milligrams of cholesterol per serving) entrée sales or the proportion of healthy entrée to total entrée sales.
Even if consumers do not immediately respond to nutrition information, mandatory labeling could still lead to improvements in consumer health if the FAFH industry reacted by improving the nutritional quality of foods sold at restaurants. For example, a FAFH labeling policy requiring disclosure of the amount of calories, fat, sodium, and cholesterol could induce restaurants’ selling products high in these ingredients to reformulate their product rather than risk losing sales to restaurants’ selling nutritionally superior products. Such reformulation could alter the entire range of market offerings and precipitate better nutritional outcomes for all consumers. If consumers do not like these reformulations, restaurants will abandon them for recipes with the taste and texture that consumers prefer.
So far, the evidence on whether the 1994 act (NLEA) induced reformulation of foods consumed at home is mixed. One study that examined the snack cracker market found that the average fat content and the average share of calories from fat per serving were significantly lower in the post-NLEA period compared with the pre-NLEA period. However, an ERS study that analyzed the nutritional quality of five product categories before and after NLEA found little change.
Since taste is usually linked to higher fat, salt, and sugar content, restaurateurs are likely to resist changing their recipes or formulating new ones unless many consumers start making different food choices. Or, restaurateurs could choose to reformulate away from one ingredient, like saturated fat, and compensate for flavor changes by boosting the sugar or salt content of the food. In this case, the overall nutritional content of a restaurant meal may not improve. Meals that are marginally lower in one or more attributes may not be much healthier than the originals.
Restaurants could also respond to mandatory labeling by expanding their menu options to include healthier choices, while still selling or even promoting their less healthy options. In this way they could satisfy their nutritionally conscientious customers without alienating their customers who prefer higher fat or caloric foods. This strategy could lead to unintended outcomes for nutrition information policy. A study by Christine Moorman of Duke University showed that following NLEA, food suppliers expanded price promotion of nutritionally poorer brands while promotion of nutritionally better brands did not change significantly between the two periods.
A Tax on Snack Food
Another proposal to reduce obesity in the United States is a tax on snack foods that are high in salt, added sugar, fat, and calories. As consumers substitute healthier foods, their weight would fall and their health would likely improve. (Some variations of this proposal would use revenues raised from the tax to fund expanded nutrition education programs.)
Selective taxation of particular foods is rare for the Federal Government. Oleomargarine was taxed from 1886 until 1950, and during two periods in the early part of the 20th century, the Federal Government taxed soft drinks. Thus, a Federal snack food tax would be novel from a fiscal perspective.
For those consumers who are not overweight and enjoy snack foods, there are only costs associated with the tax. They would either pay the tax on their favorite snack foods or choose a less satisfying diet. Also, excise taxes on food tend to be regressive—the burden of the tax would likely fall disproportionately on low-income consumers, who spend more of their income on food than do middle- or upper-income consumers.
The health benefits of the tax depend on how big an incentive the tax is for consumers to avoid taxed foods and make better dietary choices. Imposing the tax may not create a strong incentive for consumers to make changes. First, to influence consumer choices, the tax must be passed on to retail consumers. Sometimes manufacturers absorb the entire tax, leaving retail prices and consumers’ behavior unchanged. If snack food companies operate in competitive markets, the tax would be passed on to consumers because the companies are paying competitive prices for their inputs and cannot push the tax onto suppliers. When food suppliers have some ability to set prices, the relation between taxes and retail prices is less direct.
| Snacks | Share of households that purchased snacks (percent) | Average quantity purchased by households that did purchase (pounds) | Per capita quantity purchased by households that did purchase (pounds) | Household expenditure by households that did purchase (dollars) |
|---|---|---|---|---|
| Potato chips | 91.3 | 9.76 | 4.18 | 26.14 |
| All chips | 95.5 | 16.34 | 7.00 | 41.43 |
| Other salty snacks | 96.8 | 16.47 | 7.92 | 37.41 |
| All salty snacks | 99.2 | 31.81 | 14.47 | 76.39 |
| Source: Tabulated by ERS from ACNielsen Homescan panel, 1999. | ||||
Second, the tax base—the foods that are taxed—has to be sufficiently broad to induce better choices. The tax base has to include nutritionally equivalent foods, however infrequently the latter are consumed. No benefits accrue if the tax simply induces substituting one snack food for another—pork rinds for potato chips. Many economists have studied demands for broad classes of foods (for example, substitution among beef, pork, chicken, and fish). How consumers might substitute away from particular types of highly processed food is not yet clear. Tax proponents might hope that consumers would substitute fruit and vegetables for snack food.
Third, consumers would have to respond to changes in retail prices. Looking at household expenditures in relation to income reveals that consumers are unlikely to be greatly influenced by a tax. Household expenditures on the entire class of salty snack foods (chips, nuts, pretzels, cheese puffs, and popcorn) are for most households about 0.1 percent of annual income. Consumers are not likely to pay much attention to changing retail prices for small expenditures. Other goods, like homes and cars, will command much more of their interest in prices.
ERS research estimating household demand for snack foods confirms that salty snack foods are not very responsive to prices. Estimated price responsiveness was similar in magnitude to that found in other empirical research for cigarettes and alcoholic beverages. That is, price increases may reduce purchases, but the reduction will be much smaller than the tax-induced price increase. A relatively small tax on snack food, say 1 percent, would have vanishingly small impacts on dietary choices and thus negligible impacts on weight or health. Since calculations were made under the assumption that the entire tax would be passed forward, the actual impacts may be smaller still.
Higher tax rates, say 30 percent, appear to influence consumer food choices and weight so long as the tax base is broad. But such results are tentative since the full range of consumer substitution possibilities is difficult to model and may not correspond to previously observed consumption patterns.
Curtail Food Advertising, Particularly to Children
Some health researchers and health policy activists have recommended placing restrictions on food advertising. Some have proposed eliminating ads for candy, soft drinks, fast foods, and sugared cereal aimed at children. Proponents argue that these restrictions will help improve children’s health. If children were no longer exposed to frequently repeated advertisements, other foods could compete for their attention. The effectiveness of a policy curtailing food advertising to children depends on the extent to which food ads alter children’s preferences for different food groups or simply shift them from one hamburger chain (and one toy) to another. If advertising is effective at forming children’s food tastes and preferences, health benefits may accrue from minimizing children’s exposure to advertising.
The food industry spends enormous amounts on advertising; however, it is not clear to what extent these expenditures increase overall calorie consumption or how much consumption would drop if advertising expenditures were curtailed. Little direct evidence links food advertising and overall diet quality. Studies that link the demand for individual food products and advertising are legion—many show that advertising does increase sales, and some show that advertising is cost-effective. Even generic advertising studies usually show demand increases in response to such expenditures. But, because food encompasses many products and varieties, increasing demand for one food or even a class of foods says very little about overall diet quality.
Evidence from the cigarette industry—where advertising has been restricted—offers some insights. Numerous studies, though ongoing, largely conclude that aggregate cigarette advertising has a small or negligible impact on overall cigarette smoking. Promotional expenditures sway consumers from one cigarette brand to another, leaving the number of smokers and the number of cigarettes smoked unchanged. If advertising affects food consumers similarly, then restrictions on food advertising may have a larger impact on brand choices than on overall food groups consumed or diet quality. Food markets, for the most part, have stable aggregate demand, and advertising levels are strategically used to maintain market or brand share.
Additional evidence from cigarette market studies suggests, however, that advertising effects may be different for children. Cigarette advertising is effective in getting children’s attention, and children’s recall of the ads is correlated with smoking behavior or initiation. For children, cigarette advertising may be more inducement than brand identification.
Potential benefits of restricted food advertising could be complicated in that across-the-board restrictions could result in lower prices and increased consumption of foods bearing the advertising restriction. Some studies found that aggregate cigarette consumption actually increased after the U.S. banned broadcast cigarette advertising. Cigarette companies, no longer allowed to compete through broadcast commercials, were forced to compete more on price, and were able to do so from advertising savings. If restrictions on food advertisements have similar effects on price and consumption, then Americans could end up fatter, not fitter.
Can Policies Reduce Obesity Rates?
Weight status—underweight, healthy weight, overweight, or obese—is, for most people, an outcome of personal choices: what and how much to eat and whether and how much to exercise. Changes in habits are possible—recent statistics from the Centers for Disease Control and Prevention indicate that former smokers now outnumber smokers. Furthermore, habits would not have to change drastically to lead to reclassifying the weight status of most Americans. The American Dietetic Association says that each additional 3,500 calories a person consumes results in an additional pound of body weight. That implies that a person who gave up 100 calories (equivalent to a piece of toast) each day for a year would end up approximately 10 pounds lighter at year’s end.
The list of policies that could potentially help Americans turn the corner on obesity and overweight is as long as the list of factors that influence an individual’s diet and lifestyle choices. The list of unintended consequences stemming from obesity policy is probably longer. Even the most apparently straightforward policy proposal can have surprising effects: mandatory nutrition information at fast food restaurants could lead to reformulations or price promotions that do not necessarily contribute to healthier diets; taxes on snack foods could lead some consumers to substitute equally unhealthy foods for the taxed food; and restrictions on food advertising could ultimately lead to lower prices for food subject to the restrictions. Food policy overflows with unintended consequences. The trick is making sure they do not overwhelm the intended ones.
This article is drawn from:
- Variyam, J. (2005, February 1). The Price is Right: Economics and the Rise in Obesity. Amber Waves, U.S. Department of Agriculture, Economic Research Service.
- Variyam, J. (2005). Nutrition Labeling in the Food-Away-From-Home Sector: An Economic Assessment. U.S. Department of Agriculture, Economic Research Service. ERR-4.
- Is There a Role for Government in Reducing the Prevalence of Overweight and Obesity?. (2004). Choices, pp. 41-45. by Fred Kuchler and Elise Golan.
- Societal Costs of Obesity: How Can We Assess When Federal Interventions Will Pay. (2002). USDA, Economic Research Service. Food Review, 25(3):21-27.
- Taxing Snack Foods: What to Expect for Diet and Tax Revenues. (2004). AIB-747-08, USDA, Economic Research Service. by Fred Kuchler, Abebayehu Tegene, and J. Michael Harris.